Case-Based Learning in Radiology: Complete Guide for Medical Educators [2025]
The Challenge: Why Traditional Radiology Teaching Falls Short
Teaching radiology to medical students is a challenging task. Instructors spend hours creating slide presentations that students will quickly forget, since static images fail to convey the complexity of real diagnostic work. Managing and sharing medical imaging files across multiple devices becomes a technical nightmare. Above all, it is difficult to motivate students to learn concepts without hands-on experience.
What is Case-Based Learning in Radiology?
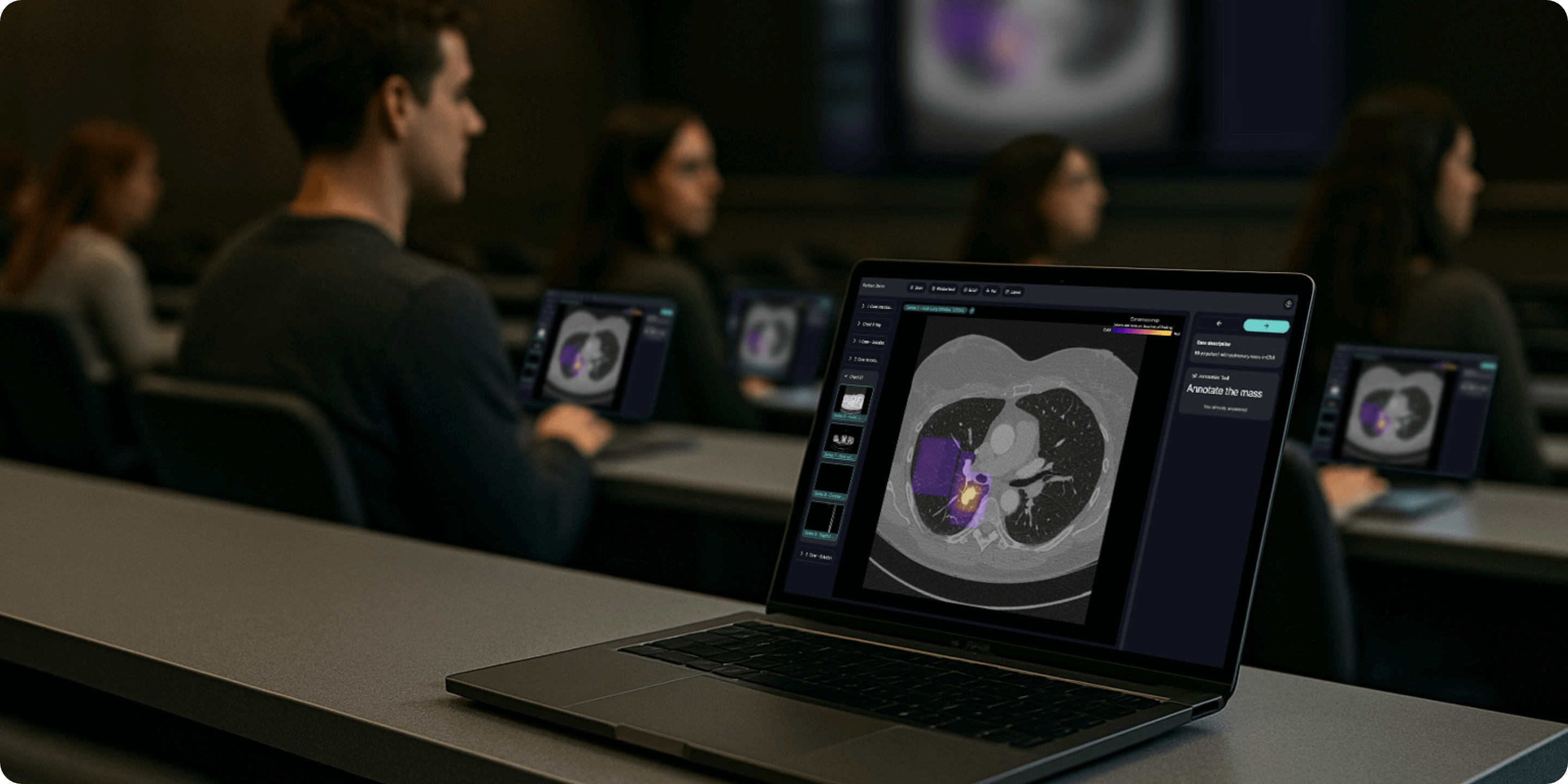
Case-based learning (CBL) uses real medical images to teach students how to think like radiologists. Instead of sitting through passive lectures, students work with actual clinical cases that mirror daily practice. They examine images using a medical imaging education software, suggest possible diagnoses, and explain their reasoning while an instructor guides them through the diagnostic process. This approach combines anatomy, disease patterns, clinical context, and reporting skills into one integrated learning experience. [1,2]
Benefits of CBL vs Traditional Lectures in Radiology Education
Research shows that CBL works better than traditional lectures to prepare students for clinical practice. When students actively work through radiology cases, they learn how to approach diagnostic exams and make differential diagnosis. Dealing with uncertain findings in realistic scenarios helps them learn when to call something abnormal and when to hold back. Seeing many different examples over time improves their ability to recognize patterns and tell similar-looking conditions apart. [3,4,5,6]
Why Students and Teachers Prefer CBL
Students consistently prefer CBL because sessions are interactive, clinically relevant, and provide immediate feedback. They appreciate working on problems they'll actually face in practice, like deciding when to order follow-up imaging. Getting specific feedback on their reasoning process, not just whether they got the right answer, helps them feel they're making real progress. Teachers also get better evaluations when they lead discussions, point out common mistakes, and connect imaging findings to patient care. [3,5,6] Professor Alexander Sauter, Chair of Nuclear Medicine at Stadtspital Zürich and lecturer at the University of Tübingen, improved his student satisfaction after implementing CBL with rapmed.net's radiology teaching platform, demonstrating the transformative impact of interactive case-based learning.
How to Implement CBL in Radiology Courses: Time-Saving Strategies
CBL saves instructors time. Instead of creating dozens of slides, they focus on selecting fewer cases since each case is explored in depth using a DICOM teaching viewer. This significantly reduces overall preparation time, fewer slides to create, fewer cases to prepare, and less content to organize. While each case requires careful planning of the discussion, the total workload is lighter. Teachers should allow realistic time for each case (typically 5-10 minutes) to cover observation, discussion, and key learning points. [2,6]
Technical Requirements for Effective CBL
To run CBL sessions effectively and teach radiology online to medical students, you need a platform that can stream medical images to multiple devices without requiring software installation. Web-based DICOM viewers for education work best since everyone sees the same images with identical settings. The system must handle large imaging files smoothly, even on standard networks, since medical images are data-heavy and delays disrupt learning. Modern teaching platforms like rapmed.net handle these technical requirements by allowing instructors to share cases instantly with large groups, even hundreds of students on the same network, without performance issues. [1,7,8,13]
GDPR and HIPAA Compliance for Medical Image Teaching
Teaching images must be completely anonymized to protect patient privacy and comply with data protection laws like GDPR and HIPPA. This means removing all identifying information from image headers, erasing any patient details burned into the images, and removing facial features from head scans that could be used to identify someone. With a GDPR compliant radiology teaching platform like rapmed.net, you can upload DICOM images directly, and the platform automatically handles anonymization including defacing and encryption to ensure all data is processed in compliance with both GDPR and HIPAA regulations. This eliminates the time-consuming manual anonymization process while ensuring complete regulatory compliance. While properly anonymized images aren't considered personal data under GDPR, institutions should follow local policies and regularly check their anonymization process. Teaching platforms that include built-in anonymization tools, facial removal for head scans, and secure data handling help ensure compliance while reducing preparation time for instructors. [9,10,11,12]
Assessment and Feedback Tools in CBL
Including quick assessments and immediate feedback makes learning more effective and helps identify areas needing improvement. Short multiple-choice questions, reporting exercises, or key-finding identification can be inserted at decision points in a case. Immediate feedback with annotated images and example reports helps students calibrate their judgment and remember important distinguishing features. Modern PACS for medical education systems often include built-in assessment tools, for instance, rapmed.net's web-based DICOM viewer for education provides real-time quizzes and annotation exercises that help instructors identify which cases students find challenging and which concepts need more attention. [6,7,8]
Getting Started with CBL: Your Action Plan
Ready to transform your radiology teaching? How to implement case-based learning (CBL) in your curriculum
- Select your platform — Choose a web-based DICOM viewer for education that handles technical requirements.
- Start with a pilot — Test CBL with one module or rotation.
- Gather cases — Begin with 10–15 high-yield cases.
- Run your first session — Allow 5–10 minutes per case for discussion.
- Collect feedback — Use built-in assessment tools to measure impact. The shift to case-based learning represents a fundamental improvement in how we teach radiology to medical students. By addressing the pain points of traditional teaching methods and leveraging modern radiology teaching platforms, educators can create engaging, effective learning experiences that better prepare students for clinical practice.
References:
- European Society of Radiology (ESR). ESR statement on new approaches to undergraduate teaching in Radiology. Insights into Imaging, 2019;10:109. DOI: 10.1186/s13244-019-0804-9. Reference Link
- Sugi MD. Interactive, case-based learning in radiology education. Abdominal Radiology (NY), 2021. DOI: 10.1007/s00261-021-03147-z. Reference Link
- Wachsman U, et al. The impact of interactive clinically-based learning on the performance of medical students in radiology. BMC Medical Education, 2023. Reference Link
- El-Ali A, Kamal F, Cabral CL, Squires JH. Comparison of Traditional and Web-Based Medical Student Teaching by Radiology Residents. Journal of the American College of Radiology (JACR), 2019;16:492–495. DOI: 10.1016/j.jacr.2018.11.031. [Reference Link]https://www.jacr.org/article/S1546-1440(18)31280-8/abstract)
- Maia D, et al. Academic Performance and Perceptions of Undergraduate Medical Students in Case-Based Learning Compared to Other Teaching Strategies: A Systematic Review with Meta-Analysis. Education Sciences, 2023;13(3):238. Reference Link
- Wade SWT, et al. What works in radiology education for medical students: a systematic review and meta-analysis. BMC Medical Education, 2024;24:???. Reference Link
- Vesselle H, et al. Development of an online authentic radiology viewing and reporting platform to test the skills of radiology trainees in Low- and Middle-Income Countries. BMC Medical Education, 2024. Reference Link
- Rita M, et al. Using PACS for teaching radiology to undergraduate medical students. BMC Medical Education, 2024. Reference Link
- DICOM Standards Committee. Security and System Management Profiles – Attribute Confidentiality Profiles (Appendix E). DICOM PS 3.15 (current). Reference Link
- GDPR Recital 26. Not applicable to anonymous data. Reference Link
- Schwarz CG, et al. Changing the face of neuroimaging research: Comparing a new MRI de-facing technique with popular alternatives. NeuroImage, 2021;231:117845. DOI: 10.1016/j.neuroimage.2021.117845. Reference Link
- Jeong YU, et al. De-Identification of Facial Features in Magnetic Resonance Images: Software Development and Validation. Journal of Medical Internet Research, 2020;22(12):e22739. Reference Link
- Pereira H, et al. Web-Based DICOM Viewers: A Survey and a Performance Evaluation. Applied Sciences, 2024. Reference Link
